Castleman disease and differential diagnosis
Published Apr 9, 2021 • By Charlotte Avril
Castleman disease is a rare non-malignant condition. It is defined by a distinctive lymph node pattern associated with clinical and biological characteristics.
There are several distinct types, both in presentation and care. To find out more, see our article "Castleman disease: Everything you need to know." Some conditions (blood disorders, autoimmune diseases, infections) may be accompanied by enlarged lymph nodes resembling those seen in Castleman disease.
What conditions are considered to be differential diagnoses of Castleman disease?
We explain below!

First of all, what is a differential diagnosis?
A differential diagnosis is a method of differentiating a disease from other conditions that have close or similar symptoms or characteristics. Its aim is to establish a more reliable diagnosis by using a methodical approach that takes into account both the elements that can exclude a condition and those that can confirm it.
How is Castleman disease diagnosed?
The diagnosis is essentially based on histological analysis conducted from a biopsy, usually of a lymph node. This type of examination consists of macro- and microscopic tissue analysis, which looks at the type of cells, whether they are cancerous or not, and their degree of aggressiveness (the grade).
Castleman disease (CD) can be defined with a number of histological features that can be seen upon histological analysis of tissue from enlarged lymph nodes:
- Follicular hyperplasia: This consists of an abnormally large volume of follicles (aggregates of lymphocytes or white blood cells) in the lymph nodes.
- Regressed germinal centers (GCs): Germinal centers are the lymph node areas in which activated B lymphocytes (white blood cells responsible for antibody production) proliferate.
- Follicular dendritic cell (FDC) prominence or dysplasia: Dendritic cells are involved in triggering immune responses. As sentinels of the body, they are used to detect pathogens such as bacteria and viruses and to activate T cells (which destroy infected cells).
- Hyalinized capillaries: Hyalinization is the destruction of collagen in the capillaries (small blood vessels), giving them a transparent, glass-like appearance.
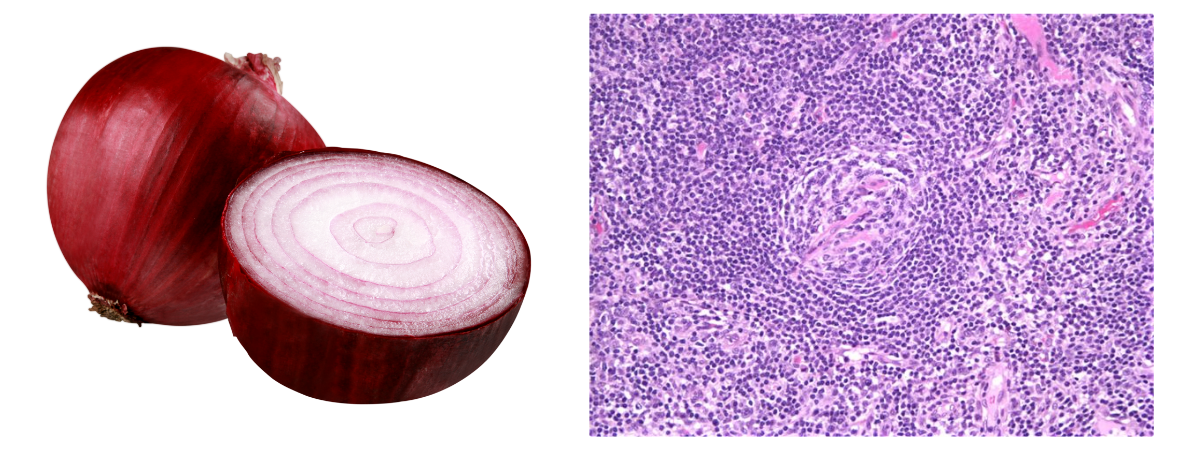
- Prominent mantle zone: In the lymph node, the mantle is the area surrounding the germinal center.
- Hypervascularity in interfollicular regions: An abnormally large volume of vessels in the space surrounding the follicles.
- Plasmacytosis: An abnormally large volume of plasma cells (cells derived from lymphocytes that actively secrete antibodies) in the space surrounding the follicles.
- Perivascular or peripheral fibrosis: Fibrosis is the abnormal change in the tissues of our body.
Some of these features can be seen in a microscope, though it is important to note that they are not unique to Castleman disease:
- An "onion skin" appearance refers to hyperplasia of the follicular mantle zone, where small lymphocytes form concentric rings
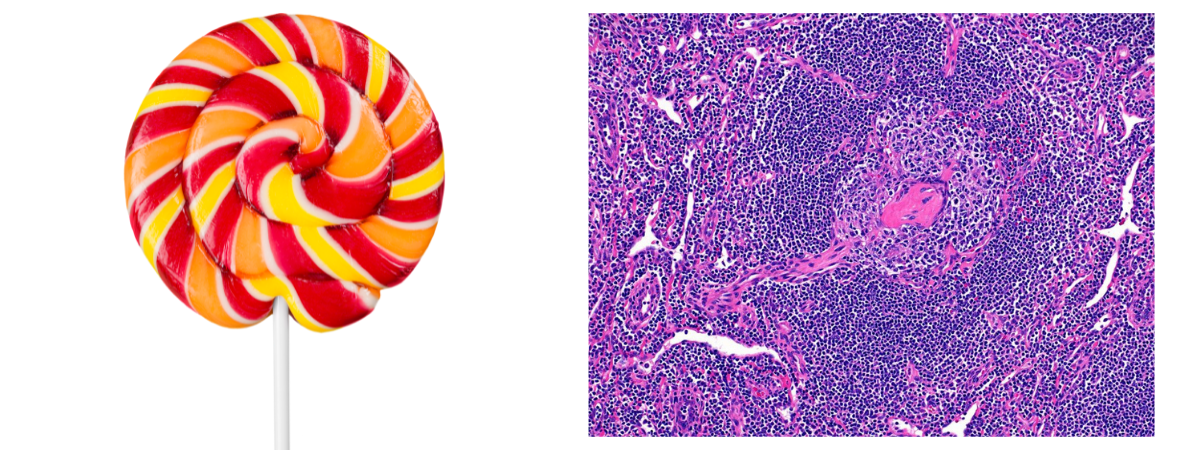
- A "lollipop" appearance refers to germinal centers penetrated by hyperplastic vessels like the stick of a lollipop.
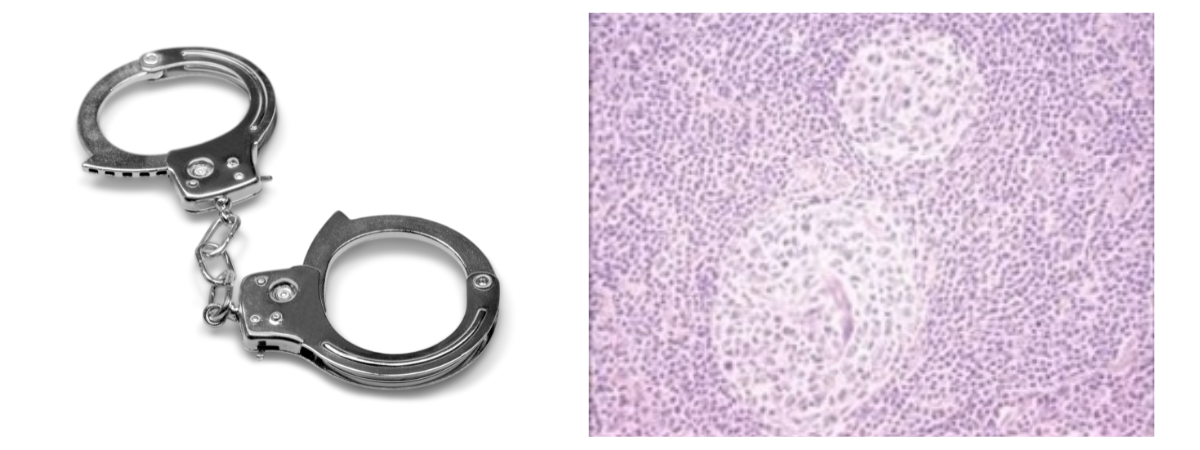
- A "budding", "twinning" or "handcuff" appearance refers to follicles that contain two or more germinal centers
In early 2017, an international panel redefined the diagnostic criteria by proposing a new histological classification for HHV-8-negative, idiopathic multicentric Castleman disease. They defined four different subtypes: hyaline-vascular or hypervascular (HV), plasmacytic (PC) or mixed, a subtype exhibiting a combination of HV or PC features. In addition to these three subtypes, there is also the form caused by the HHV-8 virus (HHV-8-positive iMCD).
What conditions should be considered in the differential diagnosis of Castleman disease?
With regard to the different types of Castleman disease (CD), the main conditions that can be considered as differential diagnoses are the following:
Malignant or tumorous conditions such as:
- Hodgkin lymphoma (HL): HL is related to the uncontrolled proliferation of abnormal B cells called Reed-Sternberg cells. It is the most important diagnosis to rule out on initial examination, especially in young adults. Castleman adenopathy (enlarged lymph nodes) and HL can co-exist in the same patient, which is why thorough examination is important.
- Non-Hodgkin lymphoma (NHL): The difference between non-Hodgkin lymphoma and HL is the presence of Reed-Sternberg cells, which are only visible in HL. This is the second diagnosis to be ruled out for the same reasons as above, particularly in the context of HHV-8 associated CD.
- Primary plasmacytoma of the lymph node: A rare disease, revealed by immunohistochemistry (IHC) (a method of detecting specific markers in tissues) which shows that the interfollicular plasma cells (cells derived from lymphocytes, actively secreting antibodies) in the enlarged lymph node are monotypic, or in other words uniform.
- POEMS syndrome: POEMS is an acronym for some of its symptoms: polyneuropathy, organomegaly, endocrinopathy, myeloma protein, and skin changes. In its classic form, POEMS can be a differential diagnosis. Some types of CD may indeed be complicated by symptoms similar to POEMS (neuropathy, skin lesions, etc.).
- Follicular dendritic cell sarcoma (FDCS): Sarcomas are a group of many cancerous tumors that develop from cells in the supporting tissue of the body. These can be tumors of the "soft tissues" (fatty tissue, muscles, vessels, etc.) or of the "hard" parts of the body (bones and cartilage).
Inflammatory or autoimmune diseases such as:
- Lupus (SLE): Lupus is an autoimmune disorder (with antibodies that attack the body) that begins with skin manifestations (lupus erythematosus) and progresses to affect various organs (systemic lupus erythematosus). It is a rare illness that can affect the skin, kidneys, joints, lungs and the nervous system. The aspect of adenopathy in SLE can sometimes be suggestive of CD. However, the diagnosis of CD is not made if lupus is established.
- Sjögren’s syndrome: Sjögren’s syndrome is an autoimmune disorder affecting less than one in 10,000 adults and is characterised by a lymphocyte infiltration in the body's moisture producing glands (salivary and lacrimal). It is responsible for dry mouth and dry eyes and for the production of various auto-antibodies. In the differential diagnosis of CD, the situation is similar to that of lupus.
- Adult-onset Still’s disease (AOSD): Adult-onset Still’s disease is a rare illness that causes inflammatory rheumatism characterised mainly by high fevers with skin rashes, with or without joint pain. Differential diagnosis in this case can be complicated by the absence of a specific marker for AOSD.
- Systemic-onset juvenile idiopathic arthritis: Systemic-onset JIA is inflammation of the joints occurring before the age of 16. Here, in the differential diagnosis with CD, the situation is similar to that of AOSD.
- Rheumatoid arthritis (RA): RA is the more frequent form of chronic inflammatory rheumatism. In active RA, the lymph nodes adjacent to the places where the arthritis occurs may have a Castleman-like appearance.
- IgG4-Related Disease (IgG4-RD): Here the question of a differential diagnosis arises because a significant number of IgG4 immunoglobulin (or antibody) secreting plasma cells are sometimes found in CD.
Infectious diseases, such as primary infections:
- Epstein-Barr virus (EBV): The Epstein-Barr virus is responsible for infectious mononucleosis (IM, also called "mono"). The adenopathy associated with IM can have similarities with CD.
- Cytomegalovirus (CMV): The cytomegalovirus is often harmless, except for immunocompromised individuals and pregnant women. The situation is similar to IM, with adenopathy resembling that found in CD.
- Human immunodeficiency virus (HIV): HIV is responsible for acquired immunodeficiency syndrome (AIDS). This situation is similar to IM with adenopathy similar to that observed in CD.
- Toxoplasma gondii (causes toxoplasmosis): The situation is similar to IM with adenopathy similar to what is found in CD.
Primary immune deficiencies, which are usually present at birth and are generally inherited genetic disorders:
- Common variable immunodeficiency (CVID): CVD is a disorder characterised by low levels of immunoglobulin (antibodies) and an increased susceptibility to infection. In certain forms, the adenopathy caused by CVID may suggest CD. Hypogammaglobulinemia (low immunoglobulin levels in the blood) can redirect the diagnosis.
- Autoimmune lymphoproliferative syndrome (ALPS): This is a rare hereditary disorder characterised by a non-malignant lymphoproliferation (abnormal multiplication of white blood cells) and a lifelong increased risk of developing Hodgkin or non-Hodgkin lymphoma. Again, the appearance of lymph nodes may suggest CD. In case of doubt, genetic analysis will confirm the diagnosis.
- Adenosine deaminase 2 deficiency: This is an auto-inflammatory disease linked to mutations in the ADA2 gene. The background is rather suggestive of systemic vasculitis (inflammation of the vessels).
The definitive diagnosis of Castleman's disease can be complicated, particularly idiopathic multicentric forms of CD. The diagnosis of Castleman's disease can only be made after a number of the tumour, infectious and inflammatory conditions mentioned above have been reviewed and excluded.
The diagnosis of Castleman's disease requires a specialist's opinion, at best in a reference centre and failing that in haematology or internal medicine.
If you would like more information on the specific diagnosis of Castleman's disease in children, please see our article: "Castleman disease in children."
For more information:
Please don't hesitate to visit the Castleman Disease Collaborative Network (CDCN) website for more information.
You can also join the Castleman disease community on Carenity to share your experience, find support and exchange information with other patients or their loved ones.
If you are interested in having your voice heard, let us know! Share your experience of Castleman disease (your diagnosis, treatments, your journey, etc.) with our members. Would you like to share your story? Feel free to send Courtney, our Community Manager, a private message or send us an email to this address: contact@carenity.us
Was this article helpful to you?
Share your thoughts and questions with the community in the comments below!
Take care!
Sources:
- Définitions d'hyperplasie, Dictionnaire médicale
- Centre germinatif, Biologie cellulaire et moléculaire
- Progeria : examen médical, Vulgaris médical
- Lymphomes à cellules du manteau, Le portail des maladies rares et des médicaments orphelins
- Définition : fibrose, Institut national du cancer
- Maladie de Castleman, HAS
- Le lymphome de Hodgkin, Gustave Roussy
- Lymphome non hodgkinien : points clés, Institut national du cancer
- Plasmocytome solitaire pulmonaire traité par radiothérapie: à propos d’un cas et revue de la littérature, NCBI
- Syndrome POEMS, orpha.net
- Définition : sarcome, Institut national du cancer
- Le lupus érythémateux systémique, Fédération des Maladies Dysimmunitaires
- Le syndrome de Gougerot-Sjögren, Fédération des Maladies Dysimmunitaires
- La maladie de Still de l’adulte, orpha.net
- Déficit immunitaire commun variable, orpha.net
- Syndrome lymphoprolifératif auto-immun, orpha.net
- Maladie de Castleman, Rare à l'écoute
Comments
You will also like

Testimonial - Castleman disease: "I was relieved to finally find out what I'd been suffering with!".
Jun 8, 2022

 Facebook
Facebook Twitter
Twitter
