What is a generic drug? How is it different from a brand-name drug?
Published Oct 2, 2020 • Updated Oct 8, 2020 • By Doriany Samair
Generics have been, since their introduction, a subject of debate, and admittedly, it's sometimes difficult to understand them!
You may have already experienced this situation: when you go to collect your usual medication, you realize that it has been replaced unexpectedly by another. And it only seems like a surprise to you! After asking the pharmacist, you learn that this is normal, that the formula is the same, but that it is for an unknown reason being produced by another laboratory which has decided that the box will be blue instead of pink. On the other hand, you are also told that if by misfortune you want the old version, you will have to pay the difference. So for two drugs that have the same effect, why should you have to pay more for one than the other?!
There's a lot to be confused about so you surely have a lot of questions. Let us explain it all to you!

What is a generic drug? How is it different from a brand-name drug?
In order to understand the concept of generic drugs, it is necessary to fully grasp the notion of what is called the “originator” or brand-name drug. To start, one must understand from what a medicine is made. There is first of all an active ingredient, of chemical or natural origin, characterized by a preventive or curative mechanism of action. This is accompanied by one or more inactive ingredients, or excipients, which are substances that facilitate the use and administration of the medicine, but which have no curative or preventive effect.
The originator drug is therefore the reference drug to which the laboratory has given a brand name and for which a patent has been filed.
Now, to introduce the generic, we shall briefly explain the life cycle of a drug.
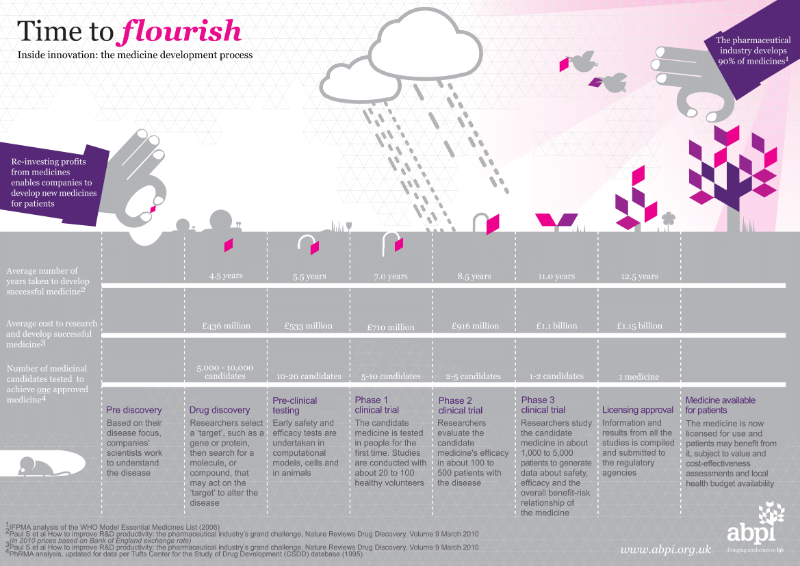
Source: https://www.abpi.org.uk/
The life of a drug begins when the laboratory registers a patent, which relies on an innovative therapeutic idea and protects it for 20 years. During this period, the laboratory prohibits any competition from conducting research in the same area. And it should also be noted that the laboratory can apply for an extension to this patent (for a maximum of 5.5 years).
During the 20 years of protection granted by the patent, the laboratory must develop its project as much as possible with the aim of marketing a new medicine, the "originator". In order to do this, a distinction can be made between 2 phases in the life cycle of the drug: the Research & Development phase, which lasts on average 10 years, and the real-life use phase of the product, a period of 5 to 10 years during which the brand-name drug is marketed.
It is important to make it clear that the first phase of R&D is crucial, as it is an experimental phase during which the laboratory carries out all the studies required by health authorities to determine the efficacy and safety of the drug's use in humans. In fact, to be placed on the market, a drug candidate must have the green light from the Food & Drug Administration (FDA), who grants the laboratory the license to market the drug. The FDA reviews the laboratory's New Drug Application (NDA) and examines all animal and human data and analyses, information about how the drug behaves in the body and is manufactured, the drug's professional labeling and manufacturing facilities.
Upon approval, prices and reimbursement rates are then negotiated in order to market the drug, which then holds a real monopoly on the market. This exclusivity leaves the laboratory a wide margin for negotiating the price, which explains the higher cost of the brand-name medicine. Indeed, the less competition there is, the higher the price will be.
Once the newly-licensed medicine is marketed, i.e. once the drug is available in pharmacies and can be prescribed to you by a doctor, the drug enters a use phase. It is important to note that this phase allows the health authorities to collect data on the medicine in terms of its safety for use by the patient, which is the role of pharmacovigilance. Indeed, a pharmaceutical product benefits from real-life national monitoring which serves as a guarantee throughout its life cycle. This monitoring consists of collecting information on the negative side effects detected. Certain adverse reactions are reported by health professionals who judge their seriousness in order to establish preventive or corrective measures. In the US, the FDA's MedWatch program is used by health professionals, patients, and consumers to report unwanted side effects of a medicine. Depending on the severity of the reported side effect, the patient information leaflet (PIL) included with the medicine may be amended, warnings may be issues or the medicine may be withdrawn from the market.
Finally, after twenty years or so, the patent expires and the compound falls into the public domain. From then on, the originator drug can be commercialized by other laboratories to market a generic drug. Sometimes, the company marketing the brand-name drug may also enter the race for generics in an attempt to keep a monopoly on a particular disease (allowing it to sell both the brand-name drug and a generic).
To fully understand the life cycle of the drug, as well as the difference between generics and originators, let's take the example of Crestor®. This is a drug in the statin class that fights high levels of cholesterol in the blood. Crestor® was originally approved in 2007, and was one of the top prescribed medications in the US in 2015, generating almost $5 billion in revenues for AstraZeneca. Its patent expired in 2012, but in 2013 Crestor® was still one of the few widely prescribed drugs that did not have a generic equivalent on the market. For obvious economic reasons, health authorities strongly encouraged the pharmaceutical industry to develop the generic equivalent of Crestor®. Today, there are at least 5 Crestor® generics available in the US.
So, what exactly is the difference between the generic drug and the brand-name drug?
What is identical between a brand-name drug and its generic:
- the generic must have the same qualitative and quantitative composition of active ingredients as the originator,
- the same galenic formulation, i.e. it must be presented in the same form: capsule, tablet, eye drops, syrup, etc.
- the same therapeutic efficacy must have been demonstrated, this is the notion of bioequivalence (ensuring that the generic has the same behavior in the body as the originator).
- the same International Non-proprietary Name (INN), i.e. the same scientific name. The INN is therefore the name of the active ingredient itself, which makes it possible, on the one hand, to identify the pharmacological class and, on the other hand, to have a common language for everyone, in order to eliminate any risk of confusion. To use the example of Crestor®, the INN of this drug is rosuvastatin. Its therapeutic family can be recognized by its suffix: -statin. Crestor®'s generic takes the name of its INN, so it's called rosuvastatin. Doctors are encouraged to prescribe it by this name, always with the aim of minimizing the risk of misunderstanding on the part of the patient.
What differs between a brand-name drug and its generic:
- The excipients, which are all the compounds of the drug other than the active ingredient(s) and are responsible for the appearance and taste of the drug.
Sometimes this difference from the originator is desirable. Syrups, for example, whether strawberry or orange-flavored, can be more or less well received depending on the patient. This is why a laboratories making generics may choose to attract new patients by extending the range of flavors.
- the NDA (New Drug Application) of a generic: generally, a complete dossier including pharmacological, toxicological and clinical data must be submitted when applying for FDA approval. However, when applying for a generic drug, the applicant can simply refer to the previous dossier submitted for the "reference" medicine and is not required to include it in their application. In addition, as for the originator, all the data relating to the quality, safety and efficacy of use are included in the NDA dossier.
For example, in the case of Crestor®, the main requirement was to prove that the generic molecule was not inferior to the originator.
Here's a term that can be frightening and is often associated with generics: "Excipients with known effects".
What does this mean?
One originator drug can lead to several generics, leaving the prescriber with a wide range of choices of medicines for the same indication. This allows him or her to personalize the patient's prescription as much as possible according to their sensitivity profile. Indeed, depending on the formulation of certain drugs, the prescriber may favor one drug over another. Among the criteria for selecting one drug over another are excipients with known effects. These are in fact excipients, i.e. inactive ingredients, but whose presence in certain patient groups requires precautions in their use. For example, in diabetics, an excipient such as sucrose should be avoided. The prescriber should therefore choose the most appropriate medicine, meeting the same therapeutic need but without sucrose.
It is interesting to mention the case of older patients, for whom it is advisable to choose a medicine that they can swallow. Thus, depending on the excipients, the size or shape of the drug may vary and be a factor or consideration for the prescriber.
Brand-name medications, like generics, are likely to contain these excipients with known effects. To learn more, you can examine a database of inactive ingredients: Inactive Ingredient Search for Approved Drug Products.
And finally, for any additional information about an originator or generic drug, you can consult the Drugs@FDA database, which lists all drugs authorized to be marketed in the US.
Why are pharmacists sometimes obligated to dispense generic medicines?
You have probably experienced the situation described above, where the pharmacist, who is supposed to dispense your usual treatment, instead gives you a medicine that you've never seen before.
First of all, let's clarify what we call pharmaceutical substitution. It is important to know that generics are divided into groups. One group contains the reference drug, which is the originator, and its generics. For Crestor® for example, we know that it has resulted in several generic drugs, all known as "rosuvastatin" but marketed by different laboratories.
Within a group, all medicines are said to be "bioequivalent". So all the medicines in the Crestor® group have the same efficacy. Watson Pharmaceuticals and Actavis, for example, have also developed their own rosuvastatin, which will be bioequivalent to each other and bioequivalent to Crestor®. This is why the pharmacist is authorized to dispense one medicine over another if they belong to the same group. Instead of the Crestor® from AstraZeneca, he or she can dispense rosuvastatin from Actavis, for example.
As you have well understood, Crestor® has been very expensive for patients and insurance companies. The development of generics has been ideal to help make medicines more affordable for consumers. So, pharmacists have been encouraged to dispense generics over brand-name drugs where possible and appropriate.
Indeed, developing a new molecule for a laboratory is a risky, long and uncertain gamble, all of which can justify the sometimes high price of the brand-name medication. When a patent expires, laboratories producing generics only have to demonstrate bioequivalence and are relieved of carrying out a number of experimental studies. This procedure then costs them less, allowing them to offer lower prices.
Is there a generic version of my brand-name medication available?
Besides asking your local pharmacist for help, the FDA has made 3 tools available to help consumers find out if a generic version of their brand-name medicine exists:
- You can use the Drugs@FDA database, a catalog of FDA-approved drugs
- You can search for generic equivalents by using the online version of the "Orange Book."
- First, search by brand name.
- Second, search again by the INN (active ingredient name).
- If other manufacturers are listed besides the brand-name manufacturer in result for searches by the "active ingredient," they are the generic product manufacturers.
- For very recent approvals, consult the First Generics List.
If you can't find a generic version of your brand-name medicine, it may be that the brand-name medicine is under patent. It is only after both patent and other periods of exclusivity are resolved that FDA can approve generic versions of the medicine.
Can I refuse to let the pharmacist give me a generic?
In general, the patient is free to choose his or her treatment, but it is important to follow a few guidelines. If the prescriber deems it medically appropriate to oppose a generic, he or she should, when writing the prescription, make sure to indicate "no substitutions", accompanied by a medical justification.
There are situations where the pharmacist can derogate from substitution without the intervention of the prescriber, in particular for medicines with a narrow therapeutic index, by indicating, in the same way as the doctor, the handwritten mention "no substitutions" and informing the prescriber.
For people aged over 75 years, for whom a change of packaging or galenic form may cause confusion and in the event of a stock shortage, the pharmacist is also authorized to dispense the branded medicine. For example, the doctor used to prescribe Crestor® to your 80-year-old father, and you absolutely do not want to change it, for fear that it will get lost with all his other pills. Since generics came on the market, the pharmacists have been encouraged to dispense generics. There are several scenarios to consider: either the doctor, aware of this, has remembered to include "no substitutions" on the prescription. In view of your father's profile, the pharmacist then has the right to dispense the Crestor®.
You should be aware, however, that some insurance companies or state aid programs will not pay, or will pay less, for a prescription if a brand-name drug is used. In this situation, you may have to pay the cost of the brand-name drug or a higher co-payment if you want the brand name drug.
Generics have long been the subject of disagreement and mistrust on the part of patients, and they remain unpopular, particularly among patients who have been taking the same treatment for a very long time.
It is important to know that these are drugs that have undergone the same battery of tests as the originator drugs before being marketed, and as such, they have an equal place in any therapeutic strategy.
Finally, in 2017, the FDA reported that generic drugs had saved the healthcare system $1.67 trillion since 2007. Today, around 90% of all prescriptions dispensed are for generics, a major step in the efforts to help make medicines more accessible and affordable for consumers.
Was this article helpful to you?
Share your thoughts and questions with the community in the comment below!
Take care!
Sources :
https://www.service-public.fr/particuliers/vosdroits/F18734
https://www.fda.gov/drugs/questions-answers/generic-drugs-questions-answers
https://www.fda.gov/patients/learn-about-drug-and-device-approvals/drug-development-process
https://www.fda.gov/drugs/buying-using-medicine-safely/generic-drugs
1 comment

You will also like

What are the dangers associated with the over-the-counter sale of certain medicines?
Dec 19, 2020 • 6 comments

 Facebook
Facebook Twitter
Twitter

