The insulin pen for diabetes: Everything you need to know!
Published Nov 14, 2021 • By Claudia Lima
As part of World Diabetes Day, and because insulin was discovered 100 years ago, in 1921, let's take a look at the means of treating the disease and especially the insulin pen.
What is the insulin pen and how does it work? Who is it designed for? How to use it properly?
We explain it all in our article!

Diabetes is an autoimmune disease, and there are two types of it: type I diabetes, or T1D, and type II diabetes, or T2D.
It is a disorder of assimilation, use and storage of sugars that come with the food. Thus, the level of blood glucose can be high (hyperglycemia) or low (hypoglycemia), which can have dangerous health consequences.
The main treatment for this condition is insulin therapy, prescribed especially for people with T1D, but also for people with T2DM, for whom first-line treatments (a balanced diet and a healthy lifestyle, as well as oral anti-diabetic treatments) are not sufficient.
The injection of insulin lowers blood sugar levels. Insulin cannot be taken orally because it will be digested, so it needs to be injected under the skin.
Different injection plans are established, depending on the type of diabetes:
- Basal insulin, with the duration of action of 24 hours, is the basic "survival" dose,
- Rapid-acting, or mealtime, insulin, as a bolus, at mealtime or to correct hyperglycemia.
There are several methods: the insulin pump, insulin syringes and the insulin pen.
Even if one of the disadvantages of the pen, as well as of the syringe, would be to have to make daily manual injections, it makes it possible not to have a special device to carry with you permanently, but to be able to easily transport your injection kit and to get the injection anywhere you want, and out of sight.
It is however necessary to be well organized and to anticipate the number of pens you would need, if they are pre-filled, or to have enough insulin cartridges to take with you.
The insulin pen
The pen is easier to use than the syringe, as it is prefilled.
There are 2 types of pens: a refillable insulin pen with a suitable insulin cartridge and a needle, and a disposable prefilled pen and a needle.
Several models of insulin pens, cartridges and needles are available. Your healthcare team can help you make the right choice. The diversity of insulin types and brands makes it possible to tailor the treatment to each patient, depending on their state of health, age, weight, height and lifestyle.
An insulin pen contains an insulin ampoule and a dial. Two different pens are used, one for basal insulin, the other for bolus insulin, due to their different chemical compositions. There are different types of insulin that can be used in different ways: rapid-acting, regular, or short-acting, intermediate-acting, long-acting and ultralong-acting.
Not all types of insulin are compatible, and insulin devices are not always covered by health insurance. Also, with this type of injection, certain rules must be followed to ensure the proper administration of insulin.
Self-injections of insulin: basic rules
It is essential to use the right method. Following certain rules can help prevent complications such as painful injections, hardened areas under the skin or poor blood sugar control.
The rules may vary depending on the material chosen, but the main ones remain the same:
- If the insulin is stored in the fridge, it must be taken out half an hour before the injection in order to be inspected,
- Check the dosage, date and type of the insulin used,
- Wash your hands thoroughly with hot water and soap,
- Remove the pen cap and disinfect the tip with 70 ° alcohol,
- Firmly insert the needle with its cap, without touching it directly, a new needle must be used for each new injection,
- Remove the needle cap,
- Test the dose by squeezing a drop of insulin (2 units) from the needle,
- Check again and select the necessary insulin dose,
- Sit comfortably in a position that leaves the skin in the injection area supple,
- Disinfect the chosen area and let it dry,
- Pinch the skin between your thumb and your forefinger to make a fold, prick and press the injection button,
- Slowly count to 10-15 after the injection is completed, without removing the needle from the skin, then gently remove it and use a cotton pad soaked in 70 ° alcohol to disinfect the area,
- Unscrew the needle, discard it in a container intended for this use and replace the pen cap.
Make sure to inject the insulin into the subcutaneous fatty tissue and not into the muscle.
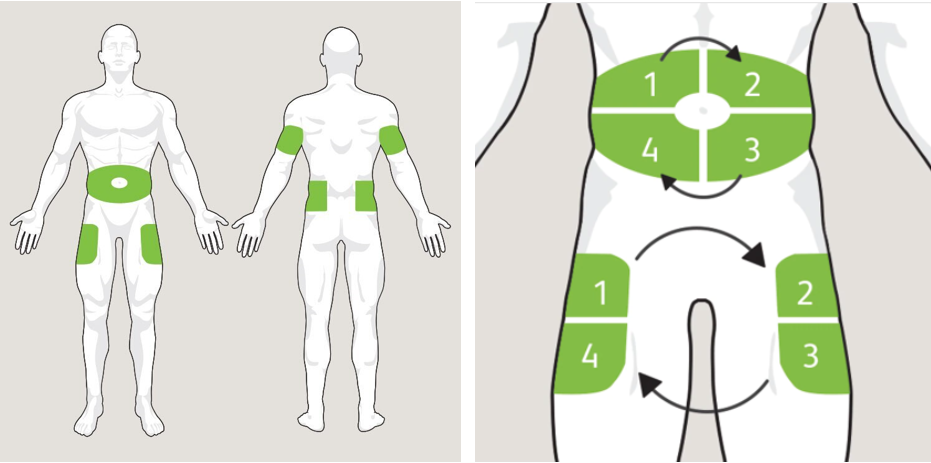
The injection can be administered to the abdomen, thighs or buttocks. Insulin is not absorbed everywhere at the same speed. In addition, it is strongly recommended to rotate the injection sites in order to avoid lipodystrophies (hardening of the tissues) and other inconveniences such as bruises, infections or inflammation.
To avoid this, it is recommended to regularly examine your skin and feel the injection sites, and in case of a doubt, to consult your doctor.
If everything is done correctly, namely: optimal injection technique, prevention of lipodystrophies and single-use needles, glycemic balance can be improved within 3 months and insulin therapy can therefore be considered the best option.
Today, to guide patients through the injection technique, medical technology company BD has made a number of helpful tutorials available on its learning center. These tutorials allow for personalized, educational guidance.
Limits of the insulin pen
Sometimes the results from using the insulin pen do not match your expectations, and here are some possible reasons:
- Blood sugar levels may be too high in the morning upon waking up, due to changing insulin needs during the night, which may not be adequately covered by basal insulin,
- Basal insulin leaves little flexibility in case of physical activity or stress, it is difficult to quickly react to the insulin needs,
- An irregular schedule is hardly compatible with basal insulin, as insulin requirements are constantly changing,
- In children, teenagers and pregnant women, self-injection of insulin does not always achieve satisfactory blood sugar levels due to hormonal fluctuations.
Insulin therapy is a lifelong treatment for type I diabetics. No matter what method of injection is used (pen, syringe, pump), it is paramount to be rigorous and to master the necessary medical procedures.
Today research is advancing, and an “artificial pancreas” developed by Diabloop, intended for type 1 diabetes meeting specific criteria, is already on the market in Europe and is reimbursed by European health systems. It consists of a subcutaneous blood sensor that evaluates blood sugar levels in real time so that the insulin pump can automatically deliver the necessary amount of treatment.
In the United States, a group of researchers at Massachusetts Institute of Technology (MIT) has designed insulin capsules capable of reaching the bloodstream. In France, med-tech company Hillo has also designed an app like many others (Glucose Buddy, MySugr, Diabetes:M, etc.) for monitoring blood sugar levels. The particularity of this application is that it uses Artificial Intelligence (AI) to predict the best blood sugar responses for each patient.
One of the latest areas of research is studying the microbiota of people with diabetes. The aim is to find out which strains of intestinal bacteria have a beneficial effect on the progression of diabetes, and then administer these strains to patients, in the form of capsules or yogurt.
Give it a like and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
Le diabète de type I, ajd-diabete.fr
Traitements du diabète : stylos ou pompe à insuline ?, dbl-diabete.fr
L'injection d'insuline, ajd-diabete.fr
Techniques d'injections avec diverses longueurs d'aiguilles, gamme.mylife-diabetescare.com
L'insuline, le traitement du diabète, federationdesdiabetiques.org
Comment utiliser un stylo à insuline, santemagazine.fr
Les bonnes pratiques de l'utilisation des stylos à insuline, diabete66.fr
14 novembre : Journée mondiale du diabète, federationdesdiabetiques.org
Technique d'injection d'insuline avec stylo, federationdesdiabetiques.org
Diabète : ces innovations qui vont changer la vie des patients, femmeactuelle.fr
Types d'insuline et usage, frdj.ca
Comments
You will also like

Fighting Schizophrenia Symptoms: a Long Journey Against Paranoia after Denial and being Admitted
Dec 12, 2018 • 6 comments

 Facebook
Facebook Twitter
Twitter

