Castleman Disease: Everything you need to know!
Published Jul 1, 2020 • By Pauline Heyries
Castleman disease is a rare disease that can occur in men and women of any age. An estimated 4,300 to 5,100 new cases per year are reported in the United States. Significant progress has been made in the classification, diagnosis and treatment of the disease since its original description by Benjamin Castleman in 1954.

What is Castleman Disease?
Castleman disease (CD) is a disorder affecting the lymph nodes and tissues, most notably with lymph node enlargement. It is neither hereditary nor communicable. It is considered lymphoproliferative, meaning that there is an overgrowth of lymphoid cells, which causes an immune system disorder. CD lies at the intersection of different therapeutic areas: hematology, oncology, rheumatology and virology.
It is a serious illness with only a 65% survival rate after 5 years (after diagnosis). This rate even drops to 40% 10 years after diagnosis. Patients with Castleman disease are also three times more likely to develop a malignant disease (like lymphoma, for example).
To date, there is no specific risk factor for Castleman disease, but studies have shown that compromised immunity may be a contributing factor. Some forms of CD are therefore associated with the herpes virus subfamily (HHV-8) or HIV.
There are different forms of Castleman disease:
At the time of its discovery, Castleman disease was categorized into 2 types: unicentric (affecting one lymph node group) or multicentric (affecting several lymph node groups). Today this classification has evolved:
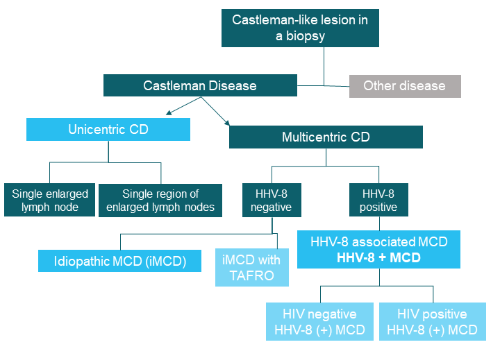
The different forms are classified according to the number of lymph nodes or regions of lymph nodes affected:
- Unicentric Castleman Disease (UCD) affects only one lymph node group or one lymph node. It is the most common, affecting 50% of cases in the general population. Additionally, it tends to affect children and young adults.
- Multicentric Castleman Disease and Idiopathic MCD (iMCD) affects multiple lymph node regions in the body. The latter is called "idiopathic" because its cause is unknown. It can occur at any age, but mature adults are often the most affected. In total, iMCD accounts for 25% of cases.
- HHV-8 associated Multicentric Castleman Disease (linked to the herpesvirus subfamily) affects adults and accounts for 8-25% of cases.
- There are other more complex and rare forms of Castleman disease but they will not be detailed in this article.
Symptoms of Castleman disease:
To better understand the symptoms of Castleman disease, it's important to understand our lymphatic system.
The lymphatic system is the set of structures that allow our immune system to function and includes different elements: organs (spleen, thymus, tonsils, lymph nodes, Peyer's patches) and lymphatic vessels that allow lymph (a fluid made of white blood cells) to circulate.
Lymph nodes play a vital role in our immune system. They filter the fluids in our body, make a variety of white blood cells called lymphocytes and prepare our body's defense cells to react specifically to viruses or a foreign body.
Patients with Unicentric Castleman disease are usually asymptomatic, they do exhibit enlarged lymph nodes (lymphadenopathy). This enlargement is generally not inflammatory or painful, however, when the nodes are very large or "misplaced", they may cause discomfort or pain.
Symptoms of MCD are varied:
- Fever and night sweats
- Fatigue
- Loss of appetite, wasting
- Nausea and vomiting
- Numbness in hands and feet
- Enlargement of liver or spleen
- Rash of red papules on the skin
- Edema (swelling), ascites (accumulation of fluid in the abdomen)
- Kidney failure
- Bruising, easy bleeding, and a risk of infection
Patients with an idiopathic multicentric form of Castleman disease (iMCD), have a clinical presentation suggestive of lymphoma which makes diagnosis difficult.
The HHV8-associated form of Castleman disease is similar to the severe forms of iMCD with some peculiarities:
- The frequency or severity of general symptoms, the presence of swelling, organ failure, the destruction of certain blood cells by other cells of the immune system, and of course Kaposi's sarcoma, which results in tumors under the skin.
- The severity of damage to blood cells and of inflammatory syndrome.
In HIV-positive patients, CD presents very similarly to what is observed in other patients but it is often more severe.
Diagnosing Castleman disease:
Since Castleman Disease is very rare, both patients and doctors often lack awareness and experience, which makes diagnosing the condition complicated. It is important to rely on clinical and biological signs as well as medical imaging. Patients must undergo thorough examinations: a physical examination and a complete blood test.
Diagnosis is based primarily on examination of the lesion (usually one or multiple lymph nodes), for which a biopsy (a minimally invasive surgical removal of a fragment of tissue or organ) is performed.
Definitive diagnosis remains difficult, in particular for iMCD and can only be made after exclusion of a certain number of tumoural, infectious or inflammatory pathologies and inclusion of a certain number of associated clinical and biological criteria.
Treatments for Castleman disease:
The chosen course of treatment depends on the form of Castleman disease.
- For Unicentric Castleman disease, standard treatment consists of surgical removal of the abnormal lymph node or lymph node region (enlarged lymph node). If all of it is removed, definitive recovery is almost certain. It is also important to note that the life expectancy of patients with UCD is not impacted.
In cases where surgery is not possible or is too invasive, radiotherapy is considered. The results are usually good, but the potential long-term risk must be considered. - For Idiopathic Multicentric Castleman disease, course of treatment is not yet well defined.
- In the first line of treatment, 2 biotherapies which target the interleukin-6 pathway (an important role in the inflammatory response) are used: siltuximab which is a monoclonal antibody and tocilizumab which is an IL-6 anti-receptor. These two treatments are effective in most patients, particularly in treating general symptoms and inflammatory syndrome. However, they are less effective for Kaposi's sarcoma.
- As a second line of treatment, conventional anti-inflammatory (corticosteroids) and immunosuppressive treatments (sirolimus, cyclosporine, rituximab) are an option.
- As a last resort, treatments targeting cytokines and inflammatory cellular pathways (bortezomib, thalidomide, anakinra) are considered.
Prognosis remains cautious and highly dependent on complications and response to treatment, but median life expectancy remains above 10 years in 70% of cases.
- For cases of HIV negative HHV-8 associated Castleman disease, standard treatment consists of an anti-B cell monoclonal antibody, rituximab, which is equivalent to chemotherapy. Relapses are possible, but patients may be responsive to the same treatment again. The prognosis here is clouded by the risk of developing non-Hodgkin's lymphoma. The median survival expectancy at 10 years is at around 50%.
- For cases of HIV positive HHV-8 associated Castleman disease, treatment is also based on rituximab. However, there are reservations about the use of this therapy. It is the most aggressive form of Castleman disease, and mortality remains high, although it has been declining in recent years. The median survival expectancy remains below 50% at 10 years.
Clinical Trials/Medical Advancements/Research
Currently, Idiopathic MCD is diagnosed when several non-specific but characteristic lymph nodes are found in patients who are also exhibiting appropriate symptoms. However, establishing an accurate diagnosis is difficult, as there are no standard criteria or biomarkers (measurable characteristics that act as an indicator of abnormality) that can be relied upon.
But, thanks to an international panel, the first diagnostic criteria for iMCD have been established, based on 244 clinical cases and 88 tissue samples. Among the major criteria are lymph node enlargement, as well as abnormalities after further medical examinations. Minor clinical criteria include increased spleen and liver size, swelling (edema), purplish papules and pulmonary symptoms, while minor biological criteria include quantitative abnormalities of red blood cells and platelets and renal dysfunction.
In addition, a study evaluating the response to siltuximab demonstrated that patients with 1 major criterion, at least 2 minor criteria and at least 1 biological abnormality responded less well to treatment than patients with at least 3 minor criteria.
Research on Castleman disease is still ongoing and studies are being conducted to improve knowledge and patient care.
How to find support on Carenity?
On Carenity you can learn more about Castleman disease through articles and group discussions.
The platform provides you with the opportunity to share your experience with other patients and find comfort, tips, encouragement and motivation to fight the disease.
Friends and family can also join and participate in the discussions, which enriches the dialogue and gives us another point of view.
Carenity allows patients and their loved ones to feel understood and supported, which is essential when living with illness. In addition to this forum, a questionnaire about Castleman disease will allow you to share your opinion on your care, your treatment path, and how you live with the condition. This information will then be used to advance research and help patients live better with Castleman disease.
For more information:
Feel free to visit the CDCN website (Castleman Disease Collaborative Network) website for more information.
Sources :
https://castleman.fr/diagnostic-et-classification-de-la-maladie/
https://www.vulgaris-medical.com/encyclopedie-medicale/lymphe-et-systeme-lymphatique
Article: “International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease” from the blood journal.
Article: “Overview of Castleman Disease” from the blood journal.
Article: “International, evidence-based consensus diagnostic criteria for HHV-8–negative/idiopathic multicentric Castleman disease ” from the blood journal.

 Facebook
Facebook Twitter
Twitter

