Is COVID-19 a respiratory illness?
Published Dec 16, 2020 • Updated Dec 18, 2020 • By Doriany Samair
COVID-19 is very much at the center of the news: every day we are confronted with an enormous amount of information. There is a proliferation of articles on the subject and never before has a disease, which was still unknown a year ago, been the subject of so many scientific publications. To keep up with this whirlwind of information and fake news, our experts enlightened us about COVID-19 at the seventh annual Carenity Scientific Committee meeting.
But what does Carenity's Scientific Committee have to say about COVID-19? How is COVID-19 a respiratory disease?
We tell you everything in our article!

Is COVID-19 a respiratory disease?
Spotlight on the physiopathology of COVID-19
Nature of the virus and description:
The virus responsible for the current global pandemic, COVID-19 (COronaVIrus Disease 2019), has the scientific name SARS-CoV-2. It belongs to the family of coronaviruses (CoV), whose name comes from the crown-like spikes on their surface, common to all the viruses of this family. They are responsible for more or less serious infections. The virus has been identified as 'SARS-CoV-2' because it is not the first of this family of viruses to infect humans. Indeed, SARS-CoV-2 refers to the coronavirus responsible for the severe acute respiratory syndrome (SARS) that was identified in China in 2002 and responsible for a deadly epidemic. Another virus of the same family was found in the Middle East in 2012, called MERS-Cov.
In fact, SARS-Cov-2 is the seventh virus of the coronavirus family to have been identified as a human pathogen, meaning it can infect the human species.
What are the signs of a respiratory disease?
Pulmonary tropism:
Figure 1. Pulmonary tropism - In vitro image of airway cells infected by SARS-Cov-2
Source: The New England Journal of Medicine - SARS-Cov-2 Infection of airway cells
For symptomatic patients, cough is the most common sign, along with fever and anosmia (loss of smell).
Through a systematic review of 148 studies conducted in 9 countries, we can list the most frequent symptoms of the disease:
- Fever 78%
- Dry cough 57%
- Anosmia 25%
- Dyspnea 23%
- Fatigue 31%
Source: SARS-COV 2,“Pathogenesis, and Advancements in Diagnostics and Treatments”.
Severe COVID-19 is represented in the diagram below, which summarizes the entire pathogenesis process.
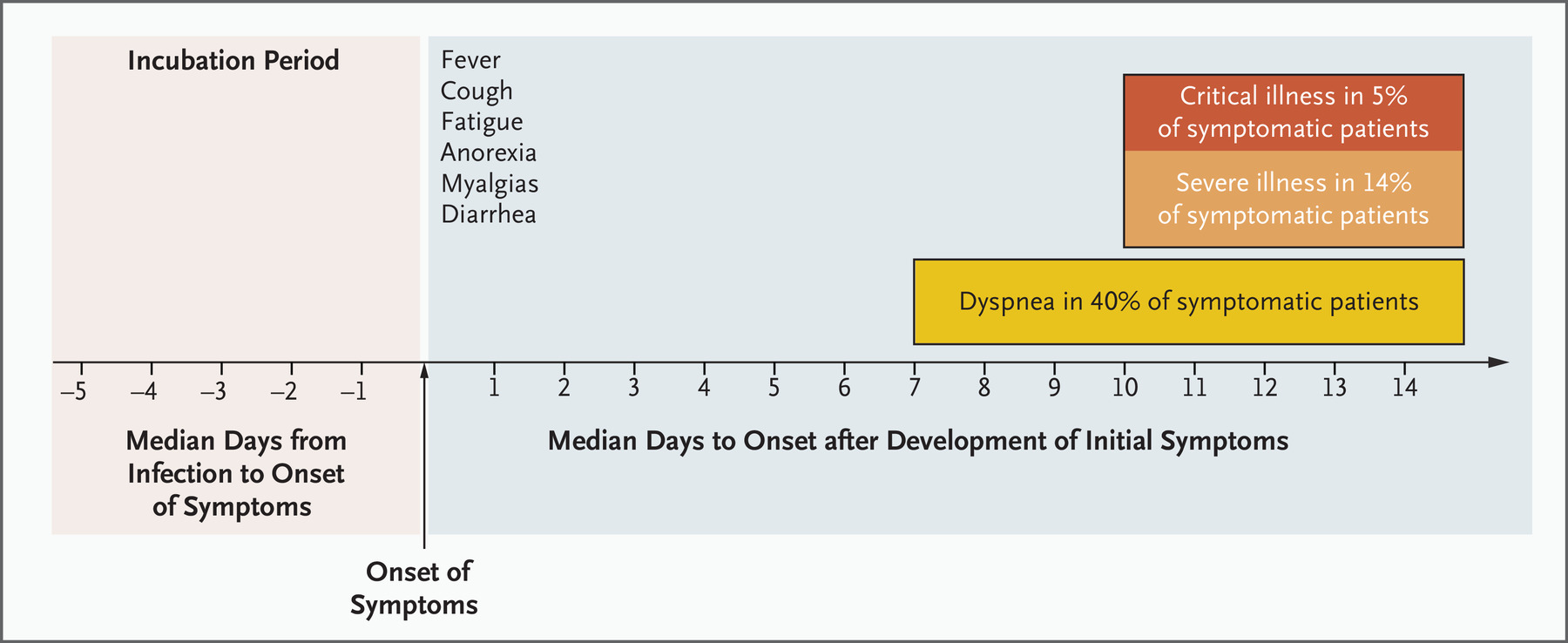
Figure 2. Severe COVID
Source: New England Journal of Medicine, 2020.
After the incubation period, there is a crucial 7-day period when the first symptoms appear. They are often flu-like symptoms, along with a cough. At the end of these 7 days, if dyspnea occurs (which is the case for about 40% of symptomatic patients), the disease is deemed severe.
COVID-19 is a particular disease since a breathless patient is a severe patient, and this is a new development for viral pneumopathies (lung infections caused by viruses). It is different from these other diseases because of its rapid evolution in which oxygen desaturation can occur suddenly.
Clinical practice reveals the existence of "happy hypoxia": the patient is out of breathe or "dyspneic" but does not necessarily alert his entourage or medical team, because he or she does not realize the seriousness of the symptom. However, this dyspneic patient could quickly find him or herself in oxygen desaturation because, without any previous warning, respiratory monitoring was not implemented. This is why hospitalization is almost automatic in the event of dyspnea: home monitoring is not adequate which explains the central and current problem of the number of beds available in the hospital.
Furthermore, among the symptomatic patients: 14% report severe illness and 5% go into intensive care.
Characteristic lung damage revealed?
Specialists have highlighted "characteristic" lung damage on X-rays. "Characteristic" means that these X-rays lead the medical team to diagnose COVID-19 in the current context. The presence of focal, bilateral, symmetrical opacities can be observed
Figure 3. Chest scan typical of COVID-19
Source: Severe COVID-19 - Source: New England Journal of Medicine, 2020.
At present, no differential diagnosis is mentioned given the high probability of being infected with COVID-19, but this could be discussed in the future when the crisis has subsided. For the time being, these images allow doctors to free themselves from a biological diagnosis, meaning the examination of biological tissues and fluids.
Frequent comorbidities
COVID-19 is a respiratory disease that does not occur primarily in respiratory patients. Indeed, pulmonologists used to think that people with asthma would be particularly impacted. In the end, they are not among the most affected - the most frequent comorbidities are in fact high blood pressure, cardiovascular disease, type 1 and 2 diabetes, kidney disease and obesity.
Respiratory illnesses come after these pathologies. This can be explained, for example, in patients with cystic fibrosis, because patients are used to respecting safety distances and measures, and protect themselves by reflex. COVID-19 is therefore a respiratory disease that does not occur in respiratory patients, in part because these patients naturally distance themselves.
Figure 4. Frequency of comorbidities
Source: Review - More than Pneumonia Distinctive Features of SARS-Cov-2 Infection. From Autopsy Findings to Clinical Implications: A Systematic Review
Lung damage with characteristic mechanisms
A fairly simple but sobering finding supported the existence of a particular mechanism in the diagnosis of COVID-19. The aim was to compare the post-mortem lungs of patients who had died of influenza with those of patients who had died of COVID-19 and to compare each with healthy lungs to extend the comparison with a control lung.
The study revealed veritable pulmonary vasculopathy (damage to the vessels of the lungs). There is in fact an intra-vascular coagulation that is limited to the lungs, meaning that thrombi (blood clots) can appear in the pulmonary capillaries. A thrombus is the result of an inappropriate and untimely coagulation. This phenomenon is probably characteristic of COVID-19 because it is not well known in other viral pulmonary illnesses, perhaps because it has not been investigated enough.
All this explains why the use of anticoagulant drugs has changed the therapeutic care of hospitalized patients. Vasculopathy is actually more significant in COVID-19 than in influenza.
The same comparative study highlighted an overexpression of genes related to vasculopathy in COVID-19 as compared to influenza. It is therefore this pulmonary vascular component, which is not necessarily found in influenza, that makes COVID-19 such a specific pathology.
A majority of asymptomatic forms
Asymptomatic forms of COVID-19 infection seem to be the most frequent: according to the INSERM, they represent 20 to 50% of infected patients. This estimation remains debatable given the difficulty in identifying these patients, who are by definition without "visible symptoms".
This observation was made in a study carried out on a Japanese cruise ship called the "Diamond Princess". There was a significant cluster on board and everyone was able to be tested and monitored.
There were 3,700 passengers on board, 712 of whom were infected and 410 were asymptomatic.
96 of the asymptomatic patients had a more thorough follow-up (tested daily with a PCR test):
- Among these, 11 developed symptoms within 4 days, showing a variability in the onset of symptoms;
- 20% had high blood pressure;
- 9% had diabetes;
This also underlines the fact that pre-existing high blood pressure or diabetes do not necessarily lead to severe cases.
- Older patients have a viral load that takes more time to become negative.
This study shows that age could be a progressive factor in viral load: older patients do not necessarily have the highest viral load, but it decreases more slowly. The older the patients are (pink curve), the likely is that they have a difficult time getting rid of the virus.
Figure 5. Crossing-Point Values in RT-PCR Testing of Asymptomatic Persons with SARS-CoV-2 Infection.
Source: Natural History of Asymptomatic SARS-COV-2 Infection
Other extra-pulmonary manifestations
COVID-19's neurological associated cases
Overall, there are few reported cases of damage to the central and peripheral nervous system, particularly in relation to the total number of patients.
- 8 reported cases of encephalitis;
- Encephalopathies are rare or non-specific;
- 3 reported cases of encephalomyelitis;
- 19 reported cases of Guillain Barré syndrome, which is viral neurological damage;
- 88 reported cases of stroke, but their true origin is not known.
However, common reported damage to the peripheral nervous system are anosmia (loss of smell) and ageusia (loss of taste), probably due to the proximity of nerve endings to the upper respiratory tract. This sort of damage is very frequent when doctors know to look for it (86%).
COVID-19's digestive and hepatic associated cases
Diarrhea is frequent found, but it remains a variable and non-specific symptom. Other digestive symptoms such as nausea, vomiting, abdominal pain or loss of appetite also occur: but these symptoms are not specifically associated with the disease and are relatively rare.
In addition, reported hepatic abnormalities are reported but are non-specific to COVID-19 and go along with the respiratory syndrome. There are also specific kidney and heart disorders described in medical literature.
How is COVID-19 treated today?
At present, there is no specific antiviral treatment for COVID-19. There are a number of ongoing studies investigating combinations of antiviral treatments.
The aim is to alleviate the symptoms in order to facilitate the natural resolution of the infection.
Nevertheless, care depends on the severity of the disease: in the hospital, oxygen therapy can be introduced to treat dyspnea, to which corticosteroids and anticoagulants are added depending on the patient's condition.
It should be noted that corticosteroids (which were distrusted at the beginning of the pandemic, particularly during the first wave) seem to be effective in the event of an acute respiratory distress syndrome (i.e. patients under mechanical ventilation, intubated and ventilated). On the other hand, corticotherapy is not effective in less severe cases. Numerous studies show that dexamethasone and hydroxycortisone significantly reduce mortality in severe cases of COVID-19. In addition, the use of anticoagulants has been shown to be effective in view of the thrombotic component of the disease.
Conclusion
In summary, COVID-19 is a respiratory illness with dominant symptoms (cough, fever, anosmia) where dyspnea is a serious factor. There are hardly any long-term after-effects on lung tissue as far as we know at present. Patients can die from respiratory failure, but it should be noted that the first lung transplant on a French COVID patient was carried out at the Foch Hospital in Suresnes, outside Paris. Very few transplants have been carried out in the world to date, only about ten.
Was this article helpful to you?
Share your thoughts and questions with the community in the comments below!
Take care!
Sources:
The article uses the literature review of Professor Antoine Magnan, former doctor and professor in the Nantes University Hospital, who recently started working at the Foch Hospital as head of the pneumology department.
- Coronavirus et Covid-19 - "Du simple rhume au syndrome respiratoire aigu sévère" - INSERM
- "Le SRAS" - Institut Pasteur
- "Imagerie de la pneumonie COVID-19" - National Center for Biotechnology Information
- Actualités - LETTRE D’INFORMATION SUR LE COVID-19 - Société de pneumologie pédiatrique et d'allergologie
- "Natural History of Asymptomatic SARS-CoV-2 Infection" - National Center for Biotechnology Information
- "Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19" - National Center for Biotechnology Information
- Natural history of Asymptomatic SARS-COV-2 Infection
2 comments
You will also like

What are the dangers associated with the over-the-counter sale of certain medicines?
Dec 19, 2020 • 6 comments

 Facebook
Facebook Twitter
Twitter



